Experts Reach Consensus on Research Priorities
In the quest to advance Essential Tremor (ET) research that could lead to better understanding and development of successful treatments, medical professionals in the movement disorder field collaborated on a white paper published in December, 2016 entitled “Knowledge Gaps and Research Recommendations for Essential Tremor.”
 The paper developed out of a workshop these professionals attended in May 2015 and their subsequent brainstorming discussions. The non-profit ET patient advocacy organization HopeNET, which has for several years sought to connect the ET patient community to the medical research community, proudly played a role in the occurrence of the workshop, which was hosted by the National Institutes of Neurological Disease and Stroke (NINDS) in Bethesda, Maryland, USA, and included over 60 participants.
The paper developed out of a workshop these professionals attended in May 2015 and their subsequent brainstorming discussions. The non-profit ET patient advocacy organization HopeNET, which has for several years sought to connect the ET patient community to the medical research community, proudly played a role in the occurrence of the workshop, which was hosted by the National Institutes of Neurological Disease and Stroke (NINDS) in Bethesda, Maryland, USA, and included over 60 participants.
The resulting paper is a valuable guideline for the future. It is certain to be of interest to the ET community who will be glad to learn that medical professionals are indeed working to further knowledge of this movement disorder! The summary below serves as a layperson’s general overview of the detailed paper to convey information in terms that are more understandable to a general audience. Science-curious readers can pursue the paper in full through ScienceDirect here [1].
The causes of ET are poorly understood. Despite widespread occurrence, no medications have been created specifically to treat it. The goals of making ET less elusive and coordinating research efforts were driving forces behind the workshop discussions. One big challenge is limited knowledge about both the genetics and the neural pathway mechanisms involved in ET. Another has to do with inconsistencies in making an ET diagnosis. The fact that ET has multiple causes makes any simple definition of it inadequate.
Clinical research methods and approaches have been inconsistent. And without standardized procedures in place, analyses and findings disagree. The authors do an excellent job of taking an in-depth look at what they do and do not know about ET. Perhaps most importantly they take it a step further: they come to a consensus on recommendations for research in these areas: phenomenology and phenotypes, therapies/ clinical trials, physiology, pathology and genetics.
The authors recall the classic ET definition given roughly 20 years ago, as set forth by the International Parkinson and Movement Disorder Society (MDS). They mention that since that time there has been speculation about other characteristics that may need to be added to the definition such as, modest changes or abnormalities in these areas: cerebellar [2], cognitive [3] and hearing function [4, 5], plus dystonia [6].
The authors discuss how it is common for ET patients to present with new symptoms that do not fit in to the existing ET definition, changes that call into question the validity of the diagnosis. ET also appears to share overlapping features with other conditions [7]. New symptoms and overlapping features have encumbered clinicians, but they still believe a revised, workable definition is necessary clinically for the purpose of making inroads and facilitating important collaborative research.
They agree on new criteria and propose that ET going forward be considered as an isolated tremor “syndrome” rather than a single disease or condition since it has been established that ET has multiple causes.
The following are the authors’ recommended diagnostic criteria for defining ET as an “isolated tremor syndrome” in an individual:
- Bi-brachial action tremor (postural or kinetic)
- Duration of 3 years or more
- With or without head tremor or tremor in other locations
- No other diagnostic neurologic signs (e.g. overt dystonia or parkinsonism)
- No identifiable endogenous (e.g., autoimmune disease) or exogenous (e.g., toxins) disturbances that could cause tremor
- Difficulty with tandem walking is permissible, but no abnormality of gait [8]
Bi-brachial pertains to the 2 arms. Postural refers to holding a limb against gravity as in for example, holding arms out in front of the body, and kinetic refers to tremor that occurs when in action. The authors acknowledge that there are isolated tremors that do not meet the proposed ET criteria. They make clear this clinical ET definition is not meant as a detriment to continued research on other isolated tremors.
Given the absence of an identified ET gene or an identified biomarker to help with a diagnosis, emphasis is placed by the authors on gathering and classifying symptoms as fully as possible, with quality data collection and standardization efforts in place, including use of common data elements (CDEs). How is tremor measured in a clinical setting? Various tremor rating scales are used and the authors are calling for their evaluation. The rating scales include clinical assessment scales, patient-reported ratings/scales, and motion transducers, which are those devices that measure tremor amplitude or severity. Recommendations are made for development of a tremor monitor, among other technological devices. It is however pointed out that gaining insight from measuring the tremor is not as conclusive as it would seem since tremor amplitude or the severity of the oscillation can fluctuate at various times and the significance of those fluctuations is not known.
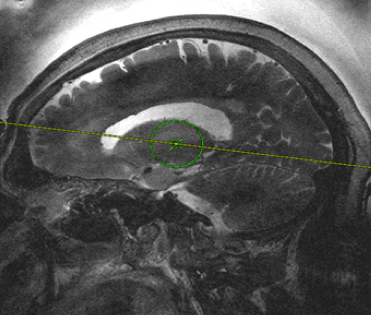
Regarding therapies or treatments for ET, the common drugs presently used were created to treat other conditions like epilepsy, high blood pressure and anxiety and were repurposed for ET when found to reduce tremor in some people. The paper explains briefly how these agents are thought to work at the cellular level. Besides the commonly used beta-blockers, anti-epilepsy drugs and benzodiazepines, clinical research has established ethanol, aka alcohol, as effective in its ability to reduce tremor amplitude for many people. Its effectiveness has led to studies in past years that isolate ethanol-related molecules such as sodium oxybate, 1-Octanol and octanoic acid, and these may turn into possible future treatments. They also seek to better understand how certain surgical interventions have met some success in reducing tremor: deep brain stimulation (DBS) and magnetic resonance focused ultrasound, both of which target and lesion the ventral intermediate nucleus (VIM) portion of the thalamus in the brain.
At the physiological level, researchers have identified a particular central nervous system circuit they think may be responsible for tremor oscillation in ET called the corticobulbocerebellothalamocortical circuit, and they are calling for investigation of it.
Genetics research findings make clear to the authors that the path to increased ET knowledge may be found in focusing on large patient cohort studies worldwide in order to make certain associations. Background is given on some important studies that have been done such as the Icelandic genome-wide association study (GWAS) that suggests the gene LINGO1 has possible associations to ET [9]. Common data elements, collection and storage of DNA bio-samples and coordinated multinational efforts are strongly encouraged.
The paper builds an awareness of scientific research being done in the ET field. The workshop provided an opportunity for experts to discuss present-day ET challenges. The authors discovered shared goals that ultimately revolve around deepening knowledge and making new treatments available, improving data, standardizing approaches, and evaluating therapies. It is a guideline for future research projects that, if adopted by researchers, could see momentum build in the direction of better outcomes for ET.
Lisa Gannon
References:
[1] F. Hopfner, D. Haubenberger, W.R. Galpern, K. Gwinn, A. Van’t Veer, S. White, …, G. Deuschl. Knowledge gaps and research recommendations for essential tremor. Parkinsonism and Related Disorders 33 (2016) 27-35. Retrieved from http://www.sciencedirect.com/science/article/pii/S1353802016303893
[2] J. Benito-Leon, A. Labiano-Fontcuberta, Linking essential tremor to the cerebellum: clinical evidence, Cerebellum 15(3)(2016) 253-262.
[3] E.D. Louis, J. Benito-Leon, S. Vega-Quiroga, F. Bermejo-Pareja, Neurological Disorders in Central Spain Study, Faster rate of cognitive decline in essential tremor cases than controls: a prospective study, Eur. J. Neurol. 17(10)(2010) 1291-1297]
[4, 5] W. G. Ondo, L. Sutton, K. Dat Vuong, D. Lai, J. Jankovic, Hearing impairment in essential tremor, Neurology 61 (8)(2003) 1093-1097.
Benito-Leon, E.D. Louis, F. Bermejo-Parmejo-Pareja, Neurological Disorders in Central Spain Study, Reported hearing impairment in essential tremor: a population based case-control study, Neuroepidemiology 29(3—4)(2007) 213-217.
[6] J. Jankovic. Essential tremor: a heterogenous disorder, Mov. Disord. 17(4)(2002) 638-644.
[7] R.J. Elble, What is essential tremor? Curr. Neurol. Neurosci. Rep. 13(6)(2013) 353.
[8] F. Hopfner, et al. Knowledge gaps and research recommendations for essential tremor. Parkinsonism and Related Disorders 33 (2016) 27-35, http://dx.doi.org/10.1016/j.parkreldis.2016.10.002
[9] H. Stefansson, S. Steinberg, H. Petursson, O. Gustafsson, I.H. Gudjonsdottir, G.A. Jonsdottir, …, K. Stefansson. Variant in the sequence of the LINGO1 gene confers risk of essential tremor. Nat. Genet. 41 (3)(2009) 277–279.



 The paper developed out of a workshop these professionals attended in May 2015 and their subsequent brainstorming discussions. The non-profit ET patient advocacy organization HopeNET, which has for several years sought to connect the ET patient community to the medical research community, proudly played a role in the occurrence of the workshop, which was hosted by the National Institutes of Neurological Disease and Stroke (NINDS) in Bethesda, Maryland, USA, and included over 60 participants.
The paper developed out of a workshop these professionals attended in May 2015 and their subsequent brainstorming discussions. The non-profit ET patient advocacy organization HopeNET, which has for several years sought to connect the ET patient community to the medical research community, proudly played a role in the occurrence of the workshop, which was hosted by the National Institutes of Neurological Disease and Stroke (NINDS) in Bethesda, Maryland, USA, and included over 60 participants. In the early 1990s, a number of companies started to offer software that was designed to convert spoken words into text that could then be displayed or printed. Among the early commercial offerings was a program entitled “Dragon Naturally Speaking”. In 1994, I tried an early version of Dragon in my workplace. After installing a microphone to my computer, I spoke several sentences rather slowly, and watched words appear on the computer monitor. Unfortunately, there were quite a few errors in the written text, and I chose to stick with keyboard entry.
In the early 1990s, a number of companies started to offer software that was designed to convert spoken words into text that could then be displayed or printed. Among the early commercial offerings was a program entitled “Dragon Naturally Speaking”. In 1994, I tried an early version of Dragon in my workplace. After installing a microphone to my computer, I spoke several sentences rather slowly, and watched words appear on the computer monitor. Unfortunately, there were quite a few errors in the written text, and I chose to stick with keyboard entry. When we founded HopeNET 5 years ago, we felt that the thing that the ET community needed most at that time was HOPE – hence the name. In the meantime, we have strived hard to bring some hope to all with ET. Accordingly, HopeNET played a key role in having the ET conference at NIH in May 2015. Since that conference, there has been a big increase on the part of industry in developing new treatments for ET. Dr. Dietrich Haubenberger of NIH is probably in the best position to know what is going on with ET. He came to the Falls Church, Virginia ET support group on October 14th and made the attached presentation,
When we founded HopeNET 5 years ago, we felt that the thing that the ET community needed most at that time was HOPE – hence the name. In the meantime, we have strived hard to bring some hope to all with ET. Accordingly, HopeNET played a key role in having the ET conference at NIH in May 2015. Since that conference, there has been a big increase on the part of industry in developing new treatments for ET. Dr. Dietrich Haubenberger of NIH is probably in the best position to know what is going on with ET. He came to the Falls Church, Virginia ET support group on October 14th and made the attached presentation,